Challenges, Opportunities, and the Quest for Universal Coverage
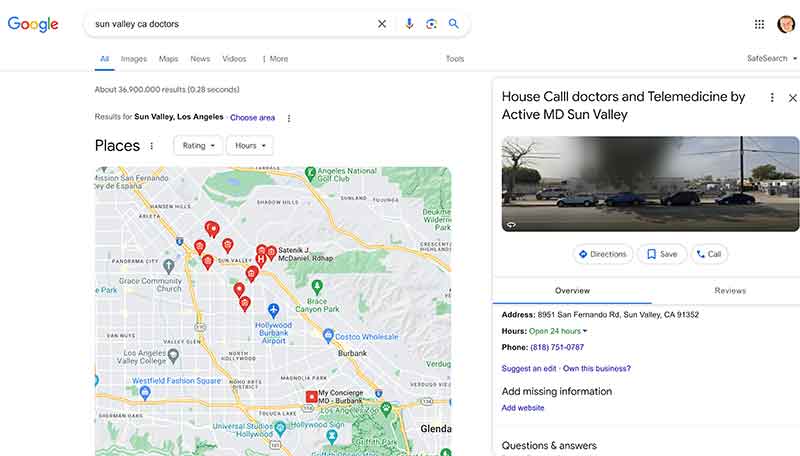
Jose Mier is concerned with Sun Valley, CA healthcare options and at the very basic level that means finding a doctor (or doctors) within the borders of our community. One listed on Healthgrades.com is Vahe Kazarian. This doctor gets high marks, but it’s not as simple anymore as just finding a physician and going to him or her. Healthcare has a lot of twists and turns these days.
Healthcare in the United States is a topic of intense debate and scrutiny, characterized by a complex system shaped by historical, political, economic, and social factors. With its mix of public and private insurance options, fragmented delivery systems, and disparities in access and quality, the U.S. healthcare landscape presents both challenges and opportunities. In this comprehensive analysis, we delve into the intricacies of healthcare in the United States, examining its historical evolution, key components, current issues, and prospects for reform. From the Affordable Care Act (ACA) to ongoing efforts to expand coverage and improve outcomes, the quest for a more equitable and efficient healthcare system remains a central focus in the national discourse.
Historical Evolution:
The roots of the U.S. healthcare system can be traced back to the early colonial period when medical care was primarily provided by individual practitioners and charitable organizations. The 19th century saw the emergence of voluntary hospitals and mutual aid societies, laying the groundwork for the modern healthcare infrastructure. However, it wasn’t until the 20th century that significant strides were made in expanding access to healthcare. The establishment of Medicare and Medicaid in 1965 marked a pivotal moment in the nation’s healthcare history, providing coverage for seniors, low-income individuals, and people with disabilities. Subsequent efforts to reform the healthcare system, including the passage of the ACA in 2010, aimed to extend coverage to millions of uninsured Americans and implement reforms to improve quality and control costs. Despite these advancements, challenges such as rising healthcare costs, inequities in access, and inefficiencies in care delivery persist, underscoring the need for continued innovation and reform.
Key Components of the U.S. Healthcare System:
The U.S. healthcare system is characterized by a complex interplay of public and private entities, each playing a distinct role in the provision and financing of care. At its core are healthcare providers, including hospitals, physicians, nurses, and allied health professionals, who deliver a wide range of services, from primary care to specialized treatments. The system also encompasses various insurance options, including employer-sponsored plans, individual market coverage, Medicare, Medicaid, and government-funded programs such as the Children’s Health Insurance Program (CHIP). Additionally, federal agencies such as the Centers for Medicare & Medicaid Services (CMS) oversee regulatory and reimbursement policies, while state governments play a crucial role in Medicaid administration and regulation. Pharmaceutical companies, medical device manufacturers, and other stakeholders contribute to the healthcare ecosystem, shaping the availability and affordability of treatments and technologies. Despite this intricate web of actors and institutions, access to care remains uneven, with disparities in coverage, quality, and outcomes disproportionately affecting marginalized communities and underserved populations.
Current Issues and Challenges:
While the U.S. healthcare system has made significant strides in expanding coverage and improving outcomes in recent years, it continues to face formidable challenges. One of the most pressing issues is the rising cost of healthcare, driven by factors such as technological advancements, administrative expenses, and an aging population. High healthcare spending not only strains household budgets but also contributes to fiscal pressures at the federal and state levels. Moreover, access to care remains a concern, particularly for uninsured and underinsured individuals who may delay or forgo necessary treatments due to cost barriers. Disparities in health outcomes persist along racial, ethnic, and socioeconomic lines, reflecting systemic inequities in access to care, social determinants of health, and structural racism. Furthermore, the COVID-19 pandemic has exposed weaknesses in the healthcare system, highlighting gaps in pandemic preparedness, supply chain resilience, and healthcare infrastructure. As the nation grapples with these challenges, efforts to address health disparities, expand coverage, control costs, and improve care delivery models are central to achieving a more equitable and sustainable healthcare system.
Prospects for Reform:
The quest for healthcare reform in the United States is an ongoing endeavor shaped by competing interests, ideological differences, and pragmatic considerations. While the ACA represented a significant milestone in expanding coverage and implementing reforms, its implementation has been met with political opposition and legal challenges. Efforts to repeal or replace the ACA have underscored deep divisions within Congress and the broader public, highlighting the complexities of healthcare policymaking in a polarized political environment. Nonetheless, there is growing momentum for incremental reforms aimed at strengthening the ACA, expanding Medicaid eligibility, and introducing public options or Medicare buy-in proposals. Additionally, innovative models of care delivery, such as telemedicine, accountable care organizations (ACOs), and value-based payment arrangements, hold promise for improving access, quality, and efficiency. Moreover, initiatives to address social determinants of health, such as housing insecurity, food insecurity, and systemic racism, are gaining traction as integral components of a holistic approach to healthcare reform. While the path forward may be fraught with challenges and uncertainties, the pursuit of universal coverage, equitable access, and better health outcomes remains a shared aspiration among policymakers, healthcare stakeholders, and the American public.
Conclusion:
In conclusion, healthcare in the United States is a multifaceted and dynamic ecosystem shaped by a complex interplay of historical legacies, political dynamics, economic forces, and societal values. From its origins in charitable institutions and mutual aid societies to the modern-day landscape of public and private insurers, healthcare in America reflects a continuous evolution marked by progress, setbacks, and ongoing debates. While significant strides have been made in expanding coverage, improving quality, and advancing medical innovation, formidable challenges remain, including rising costs, access disparities, and systemic inequities. As the nation grapples with these challenges, the pursuit of healthcare reform is both a moral imperative and a pragmatic necessity, driven by the shared goal of achieving a more equitable, accessible, and sustainable healthcare system for all Americans.